|
| |||
 |
Management of Meningiomas File 17: CEREBELLOPONTINE ANGLE MENINGIOMA
To the Introduction and Contents of Management of Cranial and Spinal Meningiomas © Congress of Neurological Surgeons
Honored Guest Presentation HTML Editor: Stephen B. Tatter, M.D., Ph.D. Disclaimer: The information and reference materials contained herein are intended solely to provide background information. They were written for an audience of physicians. They are in no way intended to constitute medical advise. For medical advise a physician must, of course, be consulted. Contents
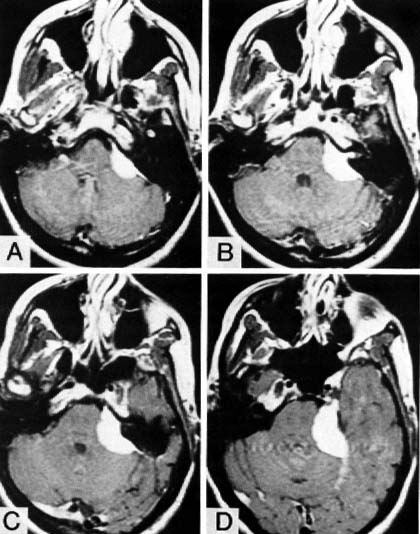
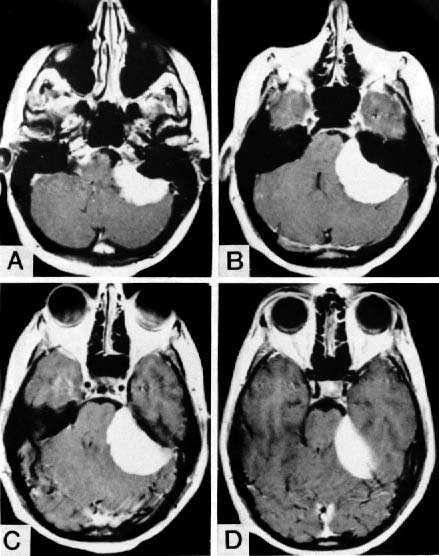
CEREBELLOPONTINE ANGLE MENINGIOMAS(Meningioma Management, File 17)ManagementThese meningiomas may arise from any area of the dura on the postelior surface of the petrous bone. At operation four general categories of tumor are found, depending on where they arise and their relationship to the seventh and eighth nerve complex:
In the past I often utilized angiography when a cerebellopontine angle meningioma was suspected. However, for most of these meningiomas it is now not necessary, because the MRI usually gives all the information needed and in most patients the blood supply comes primarily through the dural attachment. Embolization has not been a consideration. In patients with mild or minimal symptoms, an initial period of clinical evaluation and repeat scans may be indicated to determine whether there are progressive symptoms and an enlarging tumor. This is especially true in the elderly. The indications for operation are a worsening neurological deficit due to brainstem compression or cranial nerve compression. In a few patients headache or the continued presence of a stable deficit such as diplopia or hearing loss may be the indication. In this series two patients were asymptomatic. One had documented enlargement on follow-up scans and the other was concerned about the presence of the tumor. Radiation therapy has been used when there is regrowth after subtotal or radical subtotal removal and with small tumors which start to enlarge in older patients who are being observed. I use the supine position with the ipsilateral shoulder slightly elevated and the head turned to the opposite side. The details have been described (47) (see Chap. 24). This approach has worked well for visualization of the important anatomical structures, tumor removal, comfort of the operator, and avoidance of problems with air embolism or hypotension. Guthrie et al. (26) described a similar approach. Other surgeons have used the sitting position and achieved good results (58, 65, 79). The key considerations in the operation include:
ResultsThere were 57 patients with cerebellopontine angle meningiomas, 37 women and 20 men, ranging in age from 38 to 89 years, with 10 over 70 years of age (Table 17.16). In the 42 patients listed in Table 17.16, Anterior, the tumor arose anterior to the internal auditory meatus in 27 and anterior-inferior in 10 and grew diffusely in five. The extent of the tumor removal is recorded in Table 17.16. In only 14 patients could I be sure of a total removal but in another 10 a radical subtotal removal was done. On follow-up, 34 of the 42 patients had a good result, three had a fair result because of postoperative disability, four had poor results because of severe preoperative neurological disabilities that did not significantly improve, and there was one postoperative death. This occurred
None of the patients with radical subtotal removal has shown recurrence and all have been followed by scans. Most of the patients with subtotal removal had large tumors (>3 cm). Three were growing anteriorly into the middle fossa. After subtotal removal, 15 of 18 had follow-up scans, which showed no growth in eight, slight growth in five (three of whom have been given radiation therapy and two of whom are being observed after showing no further growth on subsequent scans), and moderate growth in two of the disabled patients, where nothing further has been done. Postoperative complications included permanent increased ataxia in three, one of whom had to have a cerebellar infarction removed, one patient with wound infection and meningitis, and one with a cerebrospinal fluid leak requiring repair. Several patients had temporary increases in ataxia, incoordination, or swallowing problems which improved. Four patients had a shunt for hydrocephalus at some time in their course. Of the 15 patients with meningiomas arising posterior to the internal auditory meatus, 13 had a total removal (Table 17.16). One had a radical subtotal and one a subtotal removal because of involvement of the lower cranial nerves. All had a good result. There were no postoperative neurological complications and no recurrences. Yasargil et al. (79) reported that 27 of
30 patients had a good result and in 27 the tumor was "radically
excised." Sekhar and Jannetta (65) reported total removal in 14 of
22 patients, with no operative mortality and a good outcome in 16.
Samii and Ammirati (58) reported total removal of all 24 tumors
located posterior to the internal auditory meatus, with a good
outcome for 22 patients. Of 32 patients with tumors anterior to the
internal auditory meatus, 29 had the tumors totally removed and 28
had a good outcome.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Disclaimer About Medical Information: The information and reference materials contained herein is intended solely for the information of the reader. It should not be used for treatment purposes, but rather for discussion with the patient's own physician. All visitors to this and associated sites from the Neurosurgical Service at MGH agree to read and abide by the the complete terms of legal agreement found at the Neurosurgery "disclaimer & legal agreement." See also: the MGH Disclaimer, the MGH Privacy Policy, and the MGH Interactive Program Disclaimer - © Copyright 2000. | |||
| Visitors must read the disclaimer - legal
agreement. © All Rights Reserved. Copyright © 2000 MGH Neurosurgical Service |
NeuroCare (internal access only) | ||
| System Info Contact: WebServant
or the PageServant or
e-mail C.Owen Last modified: Monday, October 7, 2002 9:47 PM | |||
| mailto:Referral@Neurosurgery.MassGeneral.org?subject=**Referral Request | |||