|
|
The motor, sensory and sundry other tracts, the spinal grey matter, and the spinal nerve roots should no longer be strangers to you. The terms and symptoms that will be discussed are used daily by clinical neurologists.
Clinicians often think in terms of "syndromes." A syndrome is a pattern of symptoms (what the patient complains about) and signs (what the physician finds) which suggest the location of a disease process and occasionally its nature. The consequence of nerve root damage (from any cause) is known as a radiculopathy (L. radicula = little root; pathos = disease), whereas the syndrome of "myelopathy"(Gr. myelos = marrow, pertaining to the spinal cord, pathos = disease) results from spinal cord damage.
Since it is impossible to discuss all types of nerve root and spinal cord disorders in the time available, we have chosen to focus on the clinical features of syndromes caused by compression by tumors or other lesions affecting the nerve roots and the spinal cord. Compression of nerve roots or the meninges covering the spinal cord usually presents with back or neck pain. Back pain is a very common symptom and results in costs up to $50 billion annually for medical care and disability payments. Back or neck pain may be caused by a variety of musculoskeletal mechanisms and the physician needs to be able to examine the nervous system to determine if there is compression of nerve roots or the spinal cord. The anatomy you are learning is essential for understanding exam findings and symptoms of root or spinal cord compression.
COMPRESSION RADICULOPATHIES
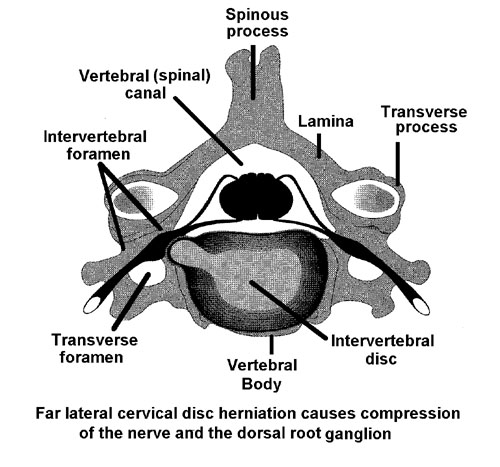
The peripheral nervous system begins at the nerve roots. Each segment of the spinal cord gives rise to a ventral or anterior motor and a dorsal or posterior sensory nerve root. The spinal nerve roots can be damaged as they traverse the spinal (vertebral) canal, but are especially vulnerable in the intervertebral foramina, where the ventral and dorsal spinal roots join to form the spinal nerves.
Look over the segmental innervation of the lower and upper limbs in the following charts. This should be familiar from your recent Gross Anatomy course and will help you understand some of the following material.
Most muscles are innervated by more than one nerve root and the lesion
of a single nerve root does not produce well-defined sensory loss because
of overlapping of the branches of dorsal root terminals from different
segments. Besides strength and sensory testing, the muscle stretch
reflexes are evaluated by briskly striking the tendon of a muscle and eliciting
a contraction, e.g. the knee jerk.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

Root compression
The hallmark of acute or chronic nerve root compression is PAIN. Pain due to nerve root compression has certain characteristics:
* it tends to follow a dermatomal distribution
* it may be accompanied by paresthesia (para, abnormal + aisthesis,
sensation, abnormal sensation such as pricking or tingling; heightened
sensitivity) or sensory loss in a dermatomal distribution
* a loss of power in the muscles innervated by the root
Back pain is one of the ten most common neurological problems seen by family practitioners.
Lumbosacral radiculopathies produce the syndrome of sciatica, cervical radiculopathies the syndrome of brachialgia. The root pain of sciatica is almost invariably accompanied or preceded by back pain (94%), and that of brachialgia by neck pain (therefore also referred to as cervico-brachialgia). Patients will, if asked to trace the pain in posterior sciatica, outline the location of the sciatic nerve "just exactly as the best anatomist". The nastiness of sciatic pain was known to Shakespeare, who employed it as a curse ("Thou cold sciatica, cripple our senators, that their limbs may halt as lamely as their manners . . . "). "The pain darts through the parts with the rapidity of lightning up and down, cutting, tearing and burning with extreme violence, increased by slight contact, or gradually becoming permanent with a gouging or crushing character." (Romberg). Superimposed on a steady, ache is a pain with a dull but biting quality, accompanied by excruciating spasms of the paravertebral and limb muscles.
The onset of root pain due to intervertebral disc herniation is often abrupt, but it may also develop over several hours or days after the start of back pain. Radicular pain is induced or aggravated by movement. Violent pain brought on by coughing or sneezing is a common complaint.
Sciatic pain usually is rather diffuse and difficult for the patient
to localize. On occasion, specific areas or points along the course
of the sciatic nerve are tender and painful. The dull pain associated
with radiculopathy is often more prominent in the proximal supply area
of the damaged nerve root. It is usually deep, referred to the muscles,
bones or joints. The sharper pain is more likely to radiate along
dermatomal boundaries.
Intervertebral disc herniation
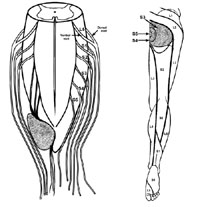
The lumbar roots emerge from below their respective vertebrae.
These roots are vulnerable just above their exit foramina, as they are
then the most ventral (anterior) and most lateral root in the vertebral
canal and lie in the immediate path of a lateral disc herniation (L5 in
the drawing on the right below). The intervertebral disc lying between
vertebrae L4 and L5 is called the L4/5 disc. The disc between the
L5 vertebrae and the sacrum is the L5/S1 disc. Since the L4 root
emerges above the L4/5 disc, a lateral herniation of the L4/5 disc damages
the L5 root. Moreover, a lateral herniation of the L5/S1 disc damages
the S1 root. KNOW THIS COLD!!
The natural history of most disc herniation is self-limited and does not require surgical therapy. One fifth of pain free people under the age of 60 have evidence of a herniated disc on MRI and 50% have evidence of a bulging disc. Hence a proper neurologic evaluation is required to define symptoms and deficits that can be linked to MRI findings. Current practice is to develop a rehabilitation program for back pain and to investigate structural causes and surgical therapies only when there is an objective neurologic deficit or pain that does not improve.
Lumbar intervertebral disc herniation occurs most commonly at
L4/5 (L5 root; 50%) and at L5/S1 (S1 root; 46.3%) interspace. Consequently,
compression of the 5th lumbar nerve root is most common, with the first
sacral nerve roots a close second.
A reason for the frequent compression of the L5 root may be the
tight fit of the L5 root in its foramen since this root has the largest
diameter and its intervertebral foramen is narrower than any other lumbar
intervertebral foramen.
Posterior sciatica
* pain which radiates along the posterior thigh and the posterolateral
aspect of the leg is due to an S1 or L5 radiculopathy (nerve roots).
When caused by S1 irritation it may proceed to the lateral aspect of the
foot; pain due to L5 radiculopathy may radiate to the dorsum of the foot
and to the large toe.
|
|
* * pain which radiates along the anterior aspect of the thigh into the anterior leg is due to L4 or L3 radiculopathy. L2 pain is antero-medial in the thigh. Pain in the groin usually arises from an L1 lesion.
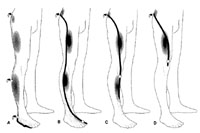
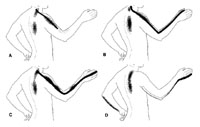
The figure above illustrates the pain distribution in lumbar radiculopathies while the figure below illustrates the pain distribution of cervical radiculopathies (click on figure for enlargement).
Because there are only 7 cervical vertebrae despite 8 cervical roots, the root number exiting between two vertebrae is always the number of the lower vertebra. For example, the C5 root exits between the C4-C5 vertebrae and would be effected by a C4/5 disc herniation; the C8 root exits between C7-T1 vertebrae and would be compressed by a C7/T1 disc.
Pain due to a C6 and C7 radiculopathy radiates from the neck and from
around the shoulder into outer aspect of the arm and forearm. C6
radiculopathy may cause pain and numbness along the dorsal aspect of the
thumb and index finger, C7 pain and paresthesia may radiate into the middle
finger.
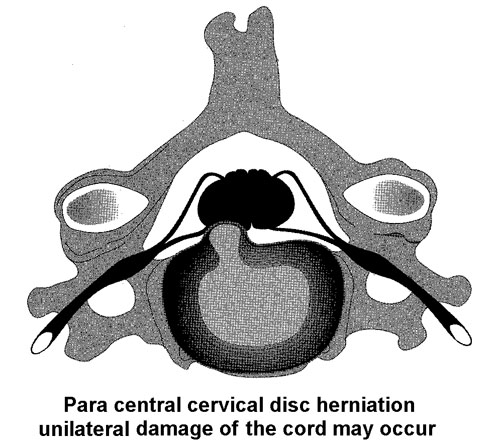
Special Cases
In the cervical and thoracic spine, intraspinal tumors, of which herniated
discs are the most common, may cause not only a radiculopathy, but may
also compress the spinal cord and the resulting syndrome is a myeloradiculopathy.
Compression of the spinal cord needs to be recognized and treated promptly.
Upper motor neuron (spasticity, Babinski sign) signs are often present
with spinal cord compression.